Health insurance brings forth more “WHYs?!” and frustrations than any other topic, and the UnitedHealthcare tragedy has revealed them all. The causes of these frustrations are bigger than any one company and touch everyone using healthcare in the U.S. Over the next few posts, we’ll explore 5 common questions:
“Do insurers profit from keeping people healthy?”
“How do insurers make profit?”
“Why do insurance companies have so much power?”
“How come there’s so little competition?”
“Why do I feel so powerless as a consumer?”
Let’s start right in with the first, likely behind much intuitive dissatisfaction … “Is it profitable for insurers to make people healthy?”
1. The one using isn’t the one choosing
Why is dissatisfaction (perhaps an understatement) with insurance so endemic? Most of the time, if consumers are unhappy with a service, they make their point by yanking their dollars, not with posterboard and markers. Why doesn’t this work in the insurance industry?

Let’s start with the most common insurance in the U.S. Employer-sponsored insurance covers about 164.7 million people, about 100 million more than covered by Medicare.[1] However, among employers offering insurance, 77 percent offer only one choice of plan.[2] Although there are dozens of U.S. insurance companies offering many types of plans, in reality, a typical employed consumer can choose one or none. Plus, the employee has no ability to leave the plan if it is not meeting his needs. At least not without quitting his job, which is usually not helpful for income- a key input to health.
On the flip side, if an enrollee felt his employer’s plan improved his health, he is equally powerless to remain in that plan if the employer, while considering its entire population and expenses, decides to switch. In a little too hilarious episode of The Office, the cowardly boss foists health plan selection onto the intense and eccentric Dwight, who “slashes benefit to the bone” to save money because “in the wild, there is no healthcare.” While I hope your HR staff considers more than lion attacks in your coverage, Dwight’s disgruntled colleagues are a mirror into an unfortunate real-life dilemma. Granted, employers may inherently want to create healthy workers, but certainly the players with the highest interest in health- the enrollees themselves—have been completely removed from the choice. No wonder the insurer ignores them!
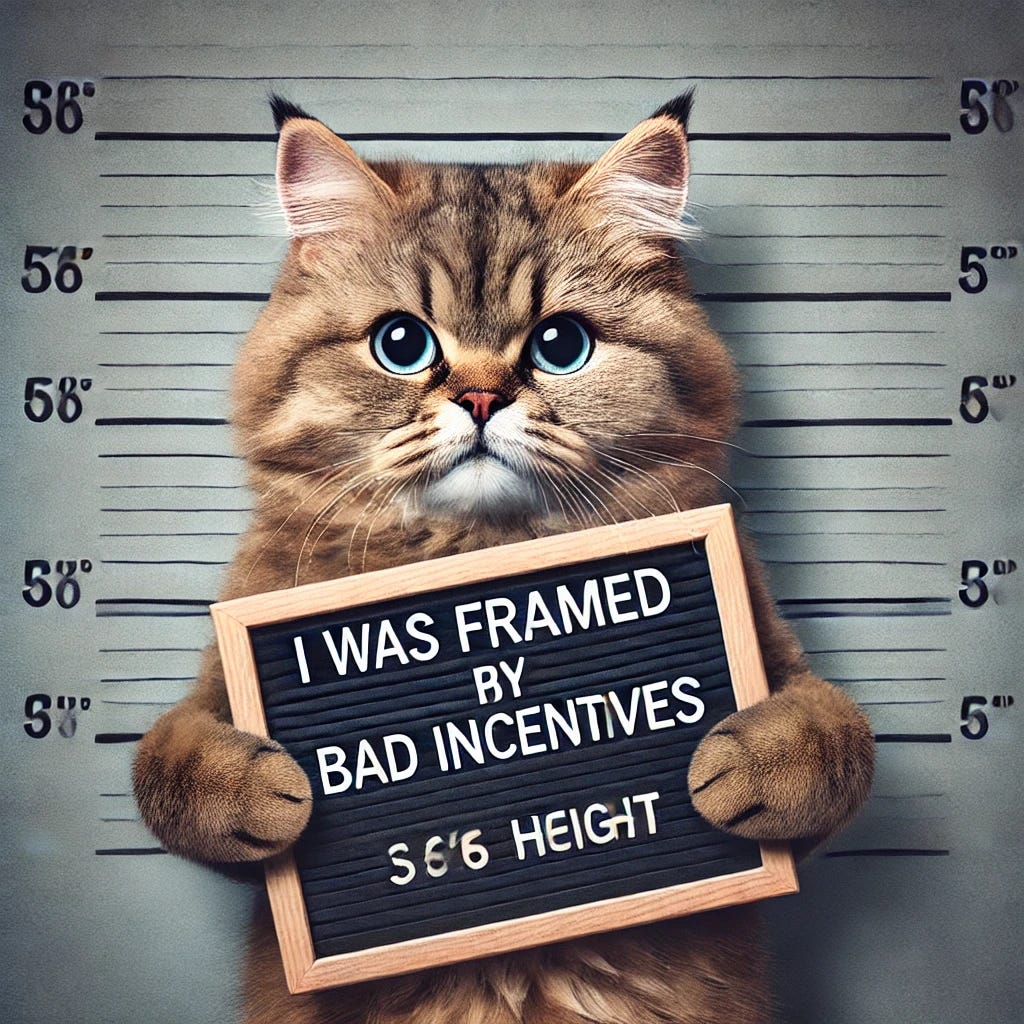
2. Prisoners to bad incentives
Creating healthy humans is a long game— preventing heart disease, managing diabetes, treating cancer—this preventive work and corrective treatment happen over many years. Unfortunately, prevention’s costs are immediate, but payoffs have long wait times, sometimes 10-20 years. In contrast, how many years of coverage do you choose during (hint) annual enrollment? Yep, only one.
This disconnect presents a problem. Any insurer who generously covers prevention and long-term curative care is unlikely to reap the rewards of this investment. If a healthy enrollee switches plans after a few years, the insurer who paid the costs ends up handing its benefits to competitors through a low-cost enrollee.
If you’re familiar with the “Prisoner’s Dilemma” (here’s my YouTube version), this might sound familiar. In this classic problem on the common good versus the individual, two prisoners want to cooperate to escape jail time, but the interrogation incentive structure leads each to ‘defect’ against their partner, leading to worse outcomes for both. When insurers can’t reap the rewards of their prevention, there’s an incentive to ‘defect’ and let distant future health be another insurer’s problem, leaving us all worse off. For example, this year’s up-to-date flu shot is standard coverage during flu season. On the other hand, basic nutrition counseling has long term benefits, but it usually only covered after a diagnosis of heart disease or Type 2 diabetes. It’s a surer bet to cut this years’ medical costs than spend to forestall future ones.
3. Who catches the hot potato?
Hold on, healthy enrollees could jump insurers, but do they do it often? In a study of over 3 million enrollees in commercial plans 2006-2018, one JAMA study found that only about 1 in 5 enrollees left in a given year.[3] Inertia from the remaining enrollees could provide a ballast for an insurer to focus on creating health. However, maintaining good health largely pays off in older ages, such as in reduced risk of heart disease or Type II diabetes, or improved mobility and cognition. Just as those preventive actions would begin to pay off around age 65, Medicare sweeps in to grab the hot potato by taking those expensive problems out of the private sector’s hands. In 2017-2020, nearly 30 percent of those 65 and older had diabetes, and their per capita health care expenditures were roughly double every other adult age group.[4] The expense of diabetes prevention is demanded of private insurance, yet the financial rewards accrue mainly to the government. Why would the insurance industry invest in creating health if they lose the prize just as it starts to pay off?[5]

If you intuitively feel that health insurance lacks sensible paths to better health, this post is to show you these frustrations are not unfounded. Beyond any individual insurance company, the structure around the industry created by public policy stacks the deck against putting consumers and their health first. In the next posts, we’ll explore how insurers make profit with an eye to how we might better align these incentives.
As always, keep me updated on what you’re up to or reach out to chat with me about these issues!
Best, TMD
[1] Overall, 60.4% of people under age 65, or about 164.7 million people, had employment-sponsored health insurance in 2023. Claxton, Gary, Rae, Matthew, and Aubrey Winger. “Employer-Sponsored Health Insurance 101: Introduction”, Kaiser Family Foundation, May 28, 2024.
[2] Kaiser Family Foundation, “2023 Employer Health Benefits Survey: Section 4: Types of Plans Offered”, Oct 18, 2023.
[3] Fang H, Frean M, Sylwestrzak G, Ukert B. Trends in Disenrollment and Reenrollment Within US Commercial Health Insurance Plans, 2006-2018. JAMA Network Open. 2022;5(2)
[4] Centers for Disease Control, National Diabetes Statistics Report: Estimates of Diabetes and Its Burden in the United States, Nov 29, 2023.
Emily D. Parker, Janice Lin, Troy Mahoney, Nwanneamaka Ume, Grace Yang, Robert A. Gabbay, Nuha A. ElSayed, Raveendhara R. Bannuru; Economic Costs of Diabetes in the U.S. in 2022. Diabetes Care 2 January 2024; 47 (1): 26–43.
[5] What if you, the individual, could be more involved? Read my post here.




That is a good question. It is difficult to assess this using any usable metrics. Most insurers seem to focus on preventive measures, annual wellness exams, and denying unnecessary testing or procedures. The denial rate ranges from vary greatly, according to a recent study with UHC at about 17% (higher than BC/BS or Elevance (former Anthem.) However, a study done about two years ago revealed that annual wellness exams are not productive, and the ROI is low. Perhaps the PAP smear, Mammograms, and colonoscopy are the highest in the ranking. Chronic illness is the major burden to insurers. Insurers are beginning to focus on nutrition and offer cash incentives but only to those below the poverty line. Although insurers are spending on marketing these aspects, how do we measure the results?